Introduction
Some of the most fascinating scientific discoveries are the most unexpected. These are the discoveries that refute the dogma, that go against long-standing beliefs, and that are fueled by a sense of curiosity and innovation. One discovery that fits into this category is the discovery of the Helicobacter pylori bacterium by Barry Marshall and Robin Warren.
The Discovery of Helicobacter pylori
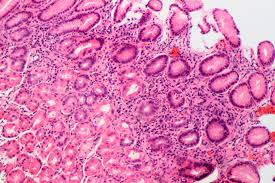
Up until the 1970’s it was a widespread belief that an excess of gastric acid and lifestyle factors, such as stress, were the causative agents of gastritis and peptic ulcer disease. However, two Australian scientists believed that there was more to the story. Robin Warren, a histopathologist, and Barry Marshall, an internal medicine student were the first to culture and propose an association between the Helicobacter pylori (H pylori) bacterium and the prevalence of these stomach ailments.
An advertisement for a cure for stomach ulcers caused by gastric hyperacidity from 1941. Image Credit: Morgan A, CC0 Public Domain.
This proposed association received much skepticism in the scientific community. The question of whether H pylori was the true cause of ulcers or simply a “bystander” that colonized the stomach mucosa after it is damaged was brought forward. Barry Marshall was so incredibly dedicated to this research that in 1985 he drank a solution of H pylori, inoculating himself with the bacterium. After 10 days he had developed flu-like symptoms indicative of gastritis, which is the precursor to an ulcer. A gastric biopsy revealed gastritis and the presence of H pylori in his stomach, proving that this bacterium was indeed the culprit behind peptic ulcers.
For their “discovery of the bacterium Helicobacter pylori and its role in gastritis and peptic ulcer disease,” Barry Marshall and Robin Warren received the 2005 Nobel Prize in Physiology or Medicine.
Helicobacter pylori Overview
Today it is known that H pylori is a gram negative, spiral shaped bacterium. This bacterium colonizes the human stomach, causing gastritis, peptic ulcer disease, and gastric adenocarcinoma. It is interesting to note that this bacterium has colonized the stomachs of approximately 50% of all humans, with a greater proportion of this prevalence occurring in countries of a lower socio-economic status. The bacterium is often acquired during childhood; however, may remain dormant and asymptomatic for much of one’s lifetime. The onset of disease caused by H pylori is influenced by the severity of inflammation, as well as the location in the stomach that is has colonized.
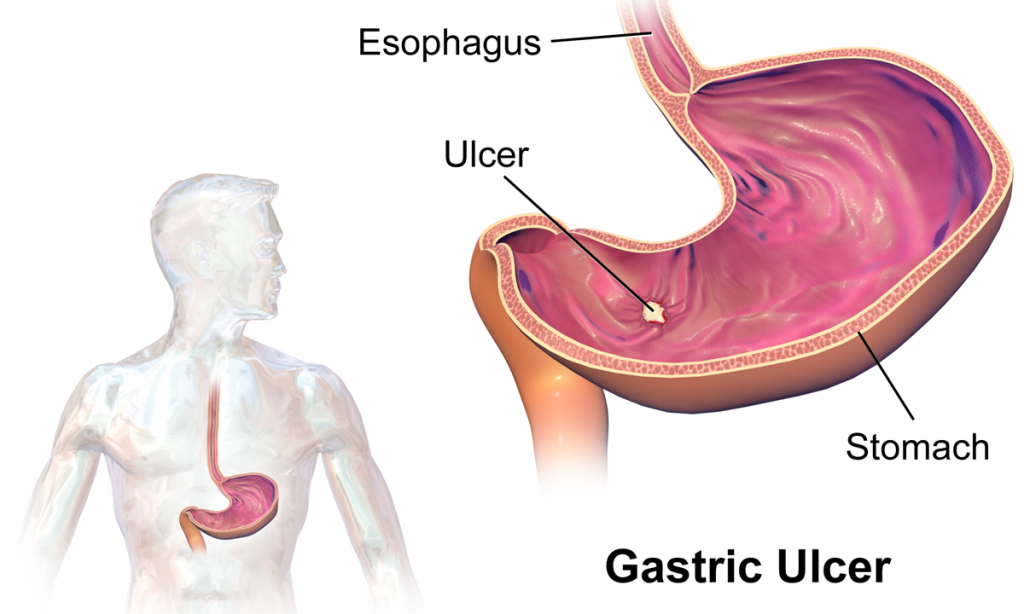
Location of the formation of a gastric ulcer. Image Credit: Blaus B, CC BY-SA 4.0.
Helicobacter pylori and Associated Malignancies
In certain cases, H pylori may infect an area of the stomach referred to as the corpus. Infection of this area results in increased and more widespread inflammation, predisposing the corpus to gastric ulcers as well as stomach carcinoma. The specific type of stomach cancer associated with H pylori colonization is called mucosa associated lymphoid tissue (MALT) lymphoma. Lymphoid tissue is not normally found in the stomach; however, is acquired in response to stimulation caused by H pylori, indicating that the infection occurs before neoplasm formation.
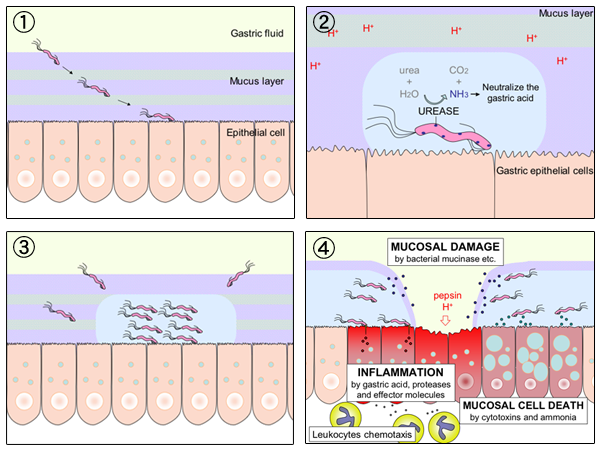
Process of colonization of Helicobacter pylori, leading to the formation of a gastric ulcer. Image credit:Tambe Y, CC BY-SA 3.0.
Steps Forward in the Treatment and Eradication of Helicobacter pylori
H pylori is a widespread bacterium in the human population; however, its prevalence has decreased and it is on its way to eradication in many countries due to improved hygiene standards and better therapeutic routines.
Antibiotics have traditionally been used to treat H pylori infections with good outcomes, provided the patient takes the correct dosage for a sufficient duration of time. More recently, H pylori has been observed to be acquiring resistance to many commonly used antibiotics including clarithromycin, metronidazole, amoxicillin, and tetracycline. The new standard for the treatment of H pylori is to use quadruple therapy, as opposed to the now ineffective triple therapy. This new quadruple therapy contains a proton pump inhibitor, bismuth, metronidazole, and tetracycline, taken for 10-14 days.
The rise in resistance of H pylori to its conventional treatments highlights the need for new and innovative therapies in order to prevent backtracking the eradications and decreased prevalence that has taken years to achieve.
Conclusions
The daring discovery of H pylori and its associated conditions was a huge milestone in the medical field. The raw curiosity and innovation exhibited by “the guinea pig doctor,” Barry Marshall, lead to retraction of the dogma of the time and an advancement in the treatment of numerous gastric ailments. The knowledge of the newfound mechanism underlying gastritis and peptic ulcers has allowed for more appropriate treatments to be developed, ultimately reducing the prevalence of these ailments world-wide. This breakthrough also revealed that a bacterium was responsible for one of the most common diseases of chronic inflammation, thus paving the way for future research concerning the role of microbes in other chronic inflammatory conditions.

Recent Comments