Have you ever tried to get into a club with a fake ID? If so, you might have more in common with a pathogen than you think. Let me explain.
The purpose of using a fake ID is to appear to be someone you aren’t- someone who is capable of entering the walls of the club to participate in the party inside. Pathogens, or disease-causing agents, also try to sneak their way past the “walls” the body has put in place to keep them out. These “walls” comprise the innate immune system. This includes physical and mechanical barriers, like the skin or mucous membranes, as well as biochemical barriers such as lysozyme, the antimicrobial enzyme found in our tears and saliva. This general mechanism does a pretty good job at keeping out most invaders. However, some pathogens are able to breach these barriers, activating an internal inflammatory response. In our analogy, say you got your fake ID from a really talented forger. If it was believable enough, you could trick the security bouncers into letting you inside the club. Once inside, there may be additional security guards who are suspicious of your presence. If they conclude that you are too young to be inside, they may work collaboratively to remove you from the premises. Similarly, once recognized as an invader, the body will work to eliminate the pathogen. It does so by attracting neutrophils, mast cells and other immune cells to the site of attack. The mast cells secrete substances that promote blood vessel dilation which facilitates the delivery of more blood and immune cells to the injured area. Neutrophils secrete substances that degrade pathogens and macrophages will subsequently eliminate the pathogen by phagocytosis. Simultaneously, the macrophages secrete cytokines at the inflammation site which attract immune system cells and activate cells involved in tissue repair.
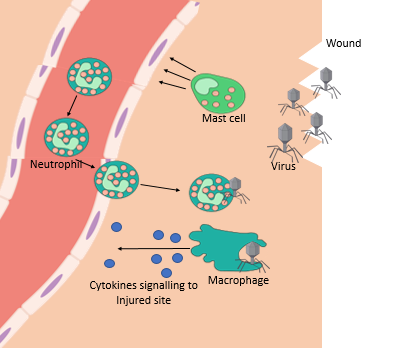
Inflammatory pathway. Constructed image by Deanna Klonarakis, clipart used include Virus photo by OpenClipart, CC0 Public Domain; Blood vessel by CRUK CC-BY 4.0; and Innate immune cells photo by Fred the Oyster, Creative Commons 4.0.
Equipped with guards, soldiers, and weapons, it sounds like our immune system is a heroic army, dedicated to keeping us alive. Although that usually seems to be the case, what if I told you that instead of providing us with safety, our immune system can actually making things worse?
Host Inflammatory Response Enhancing Severity of Infection
A recent study performed by Pingen et al. investigated the effects of mosquito saliva on the body’s response to viral infection. Two groups of mice were studied. One group was subjected to mosquito bites then subsequently injected with mosquito vectored viruses at the bite site. The second group was subjected to mosquito bites, but was not injected with the viruses. Researchers found the viral infection at the infection site was 10-fold greater in mice who received the bite and virus compared to mice who only received the virus. So, the next logical question is: how does mosquito saliva enhance infection to this level?
As it turns out, the presence of mosquito saliva at the bite site causes an inflammatory response. First, neutrophils are recruited from the blood stream to the site. Additionally, the coagulation protein system is activated, which releases substances that produce fibers to trap the virus at the site of the bite. Keeps the concentration of pathogen high at the site of inflammation, where it can be destroyed by other immune cells. The second responders, myeloid cells, arrive at the site, prepared to phagocytose the pathogen. The virus, however, has different plans for its fate. Instead of being phagocytosed, the virus manages to infect the myeloid cells, yielding them zombies, incapable of doing their intended function. The cellular machinery of the zombie myeloid cells is now dedicated to replicating the virus, increasing its population in the body.
Why Are Scientists So Interested?
The prevalence and deadliness of many diseases vectored by Aedes mosquitos, including Chikunguna disease, Zika disease, and Yellow fever, make this finding particularly relevant. The results revealed in this study suggest a new focus in preventing these mosquito vectored diseases. Researchers suggested two potential methods to reduce mosquito-vectored viral infections.
The first proposed method involves prevention of biting to prevent viral transmission. This method ideally utilizes repellants to ward off mosquitos, in conjunction with the use of prophylaxis at the bite site if repelling methods are not successful. Since research has suggested that viral particles are concentrated at the bite site, the application of prophylaxis could prove to be successful in eliminating the infection.
The second method of mosquito-vectored disease prevention includes manufacturing of a vaccine specific to mosquito salivary components. If the body builds a defense against mosquito saliva, it would not be targeted by the immune system in the case of subsequent mosquito bites. If immune cells, such as myeloid cells, are not recruited to the area, the virus would not have access to cellular machinery to exponentially grow in the body, thus suppressing its spread.
So, as is often heard, you cannot have the good without the bad. While the immune system acts as our own personal army, it also seems to play a role as an accomplice to facilitate the attack by many deadly pathogens.



Recent Comments