Introduction
Full disclosure, my title may have been a little misleading. I wholeheartedly do NOT recommend that you lose any organs! But maybe one day, if for some reason this sounds appealing to you, you will be able to do this. How you ask? Great question! The answer is stem cells.
What the Heck is a Stem Cell
Stem cells are cells that can differentiate into any other cell in the body. Embryos need these to grow. Following fertilization, all of the cells an embryo has are stem cells. They multiply a bunch so that eventually they can develop into other cells. This is important because a neuron from your brain wouldn’t be able to clear toxins in your kidneys. And that kids, is how adults are made. However, once a cell becomes, for example, a neuron, it can only ever make little neuron babies, aka daughter cells. But then, if we wiped out a population of cells we’d never be able to get it back. So how do we recover from injury? Well, it turns out that we retain some stem cells as we grow, so we can keep making all of the cells we need. That’s all fine and dandy but don’t get too excited yet. While it’s great, and frankly life-saving, that we still have stem cells as an adult, not all stem cells are the same. Embryonic, or pluripotent cells, can give rise to absolutely any type of cell in the body. On the other hand, adult, or tissue-specific stem cells, can only develop into cells from a specific tissue. On top of that, there’s a lot of ethics concerning taking stem cells from embryos. So maybe you’re losing interest about now, but do I have a plot twist for you! There’s another type of stem cell called the induced pluripotent stem cell. These cells are basically adult stem cells that have been reverted back to pluripotency. They allow researchers to use the most powerful stem cells while remaining within ethical boundaries.
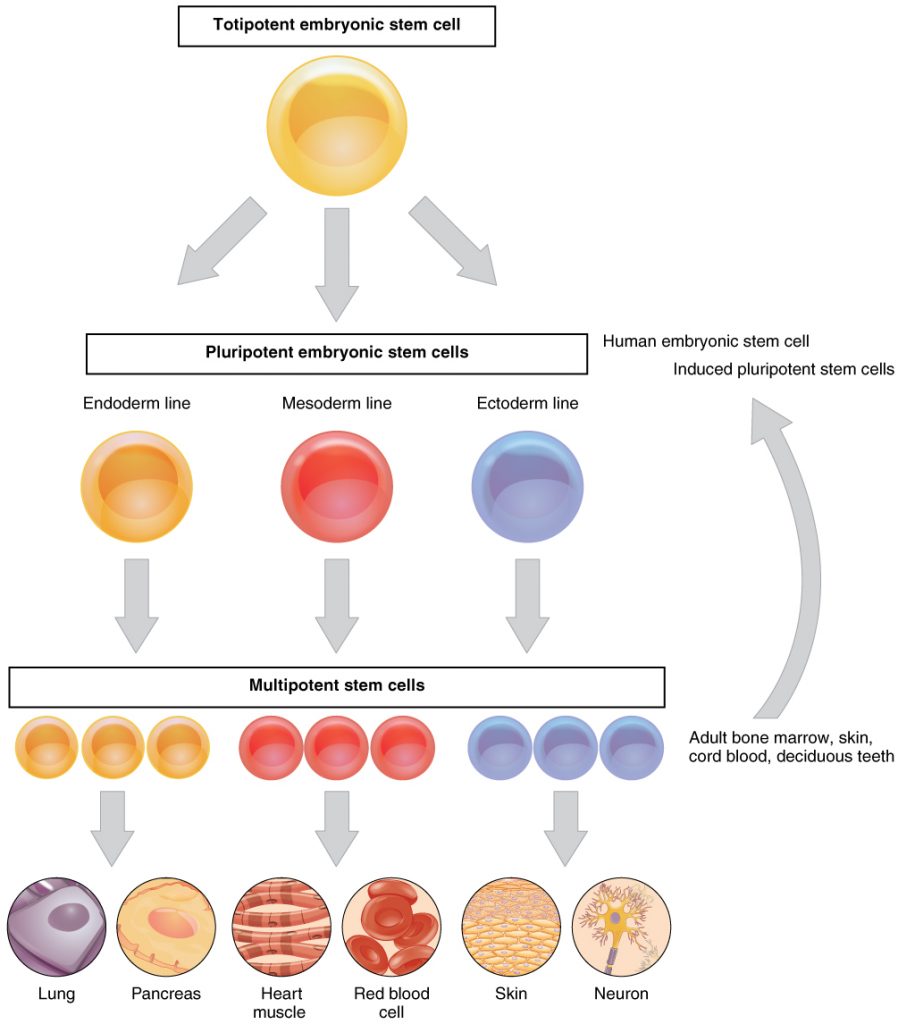
Figure 1. The different types of stem cells and what they are able to become. Image credits: OpenStax Anatomy and Physiology (author). Wikimedia Commons. Creative Commons Attribution 4.0 International license.
Let’s Get To It
Okay, let’s talk what we really want to talk about, organ regeneration or organogenesis. While this is not current practice, I’ll give you a broad overview of how it can be done, and examples of labs that have been able to do it!
There are various methods that have been created to regrow organs: single adult tissue stem cells, blastocyst complementation systems, decellularization and recellularization of bioscaffolds, and tissue engineering with stem cells. Today let’s talk about the blastocyst complementation system and the decellularization/recellularization technique. We’ll start with the blastocyst complementation system. In this method, embryonic stem cells from a donor species are injected into the genetically manipulated blastocyst of a recipient species. The recipient species is manipulated such that it will not produce a certain organ. The donor stem cells then come in, detect this deficit, and compensate for it by growing into that organ. This method is great because it allows all of the complex interactions that cells need for organogenesis. It’s also been shown to create a rat pancreas in a mouse. Now that is incredible!
Let’s move on to decellularization of matrix bioscaffolds and recellularization with stem cells. What’s important to remember with this is that to make a new heart or kidney you don’t just put some stem cells in a petri dish, throw some water and glucose over top and let them grow- cells aren’t seeds. The stem cells need an appropriate microenvironment and a bioscaffold onto which they can grow and form the correct shape. With this technique, you decellularize a donor organ (stripe it of its cells so all that remains is the structure or bioscaffold) and then you regrow the organ with stem cells. This technique was successfully used to make a functional heart in 2008. Think about that for a minute, that’s amazing!
So at this point, you should pretty much be blown away by how cool science is. But you may also be a little confused as to why this isn’t common practice if it’s as easy as it seems. Well first, my descriptions of these techniques were very simplified, they are a lot harder than they sound. Second, in the blastocyst complementation system, there are many ethical concerns regarding an inter-species technology. Ethical issues are not a small obstacle, especially considering that they can lead to legislation. In addition, using larger animal’s blastocysts has not been experimentally proven to work and needs further research. With the decellularization/recellularization technique, it’s a little hard to take someone’s heart out so you can decellularize and regrow it. Thus, while it’s great and amazing that we have found ways to grow new organs, it’s still really hard. Another complication is that it’s hard to make organs externally, aka in vitro, because cells are adapted to being inside of a body. It’s also hard to make organs internally because we can’t see everything that’s going on.
Is All Hope Lost
Worry not, all hope is not lost! With further experimentation, stem cells could very well show us a new future. So let’s end this post with some success stories! One lab was able to reconstruct complex tissues like skeletal muscles and the trachea in animal models and humans! That’s a lovely starting place for further research into the development of organs. Another lab was able to create a functional liver from induced pluripotent cells. I can already feel the excitement of undergrads with poorly functioning livers from this finding. And lastly, my favorite finding, one lab has created a printer for skin! This is huge for patients that need skin grafts, but it also has commercial applications. For example, cosmetics companies will no longer need to test on cute little bunnies. So while organogenesis is not yet here, it may be just around the corner!

Figure 2. A cute bunny who’s life may be saved by the incredible new bioprinter for skin. Image credits: CC0 Public Domain

Recent Comments