The dreaded flu season comes around every year, and along with it, a new flu shot is available. But why? Most people know that after a vaccination, your body generally becomes immune to the disease permanently. Diseases like measles, mumps, and rubella are all currently taken care of with 2 shots at a young age by the MMR vaccine, while diseases such as small pox have been complete eradicated due to the invention of vaccines. So why is it that we need a new flu vaccine every year?
To understand this, we must first understand how vaccines work in general. When a pathogen such as a bacteria, or virus, enters the body, they attack and multiply. This is called an infection and causes the symptoms of an illness, which is specific to that type of pathogen. The way the body fights back is by identifying the pathogen and then killing it. But when your immune system has never seen a new pathogen, it takes time for it to identify and produce a defensive response to deal with it. During this time the invader is able to replicate and cause damage to the body. This is where vaccines come in, they simulate an infection by giving the immune system a trial run, with a false alarm, similar to how you run fire drills in school, so in the event of a fire you are prepared and know how to respond. There are many types of vaccines such as live-attenuated vaccines, Inactivated vaccines, Toxoid vaccines, Subunit vaccines, and Conjugate vaccines(Figure 2). While they all vary in their specific mechanism of action, they do pretty much the same thing, which is to simulate an infection of a pathogen to allow the body to prepare its defences. An example of vaccine development by reverse genetics technique is show in in figure 1. Each pathogen has a coat around it called an epitope, which is specific to it and is used by the immune system to identify it. The vaccines are specific to this epitope and allow the immune system to create antibodies against it; this works in a lock and key style mechanism. Each antibody is able to recognize one epitope coat. These anti bodies are stored by memory B-cells (Plasma cells) incase of future infection by the same pathogen. Other immune cells also keep a history of infection and become memory helper T-cells and Memory killer T-cells which also respond if there is a reinfection of the same pathogen epitope. So if vaccines are so great and can create immunity against so many pathogens and even completely eradicated small pox why don’t they work against the influenza virus?
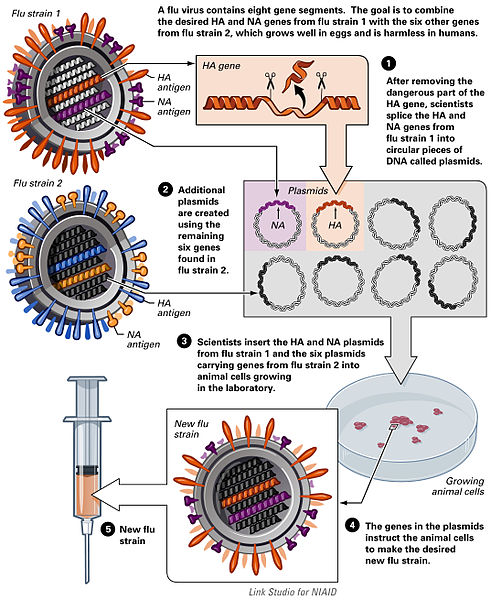
Vaccine development by reverse genetics techniques, National Institutes of Health, United States Department of Health and Human Services, Public Domian
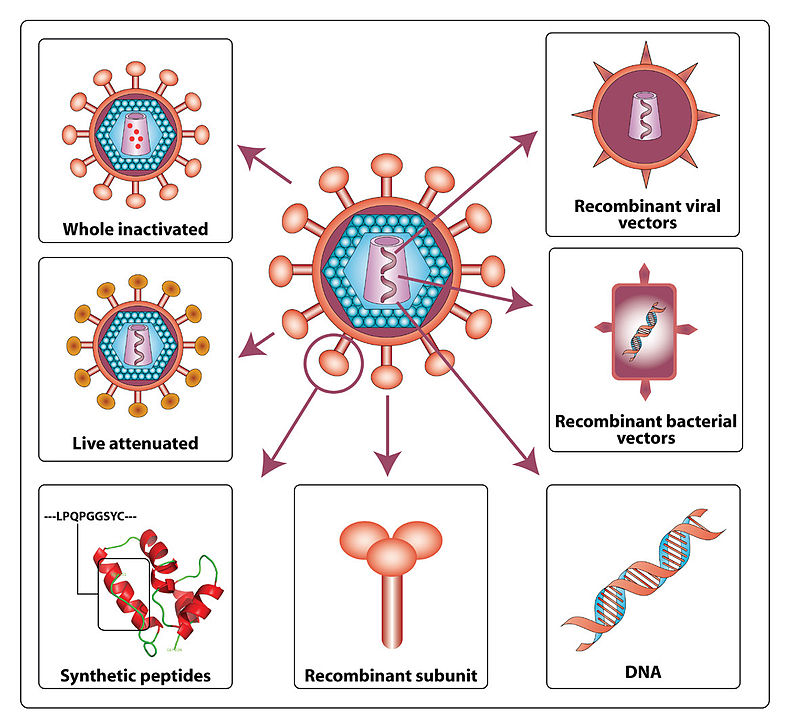
HIV vaccine strategies showing the different types of vaccines and their contents. Creative Commons Attribution 2.0 Generic – Retrieved March 3 2018.
Source: (2007). “Pathogenicity and immunogenicity of attenuated, nef-deleted HIV-1 strains in vivo”. Retrovirology 4: 66. DOI:10.1186/1742-4690-4-66. PMID 17888184. PMC: 2075523
Author: Gorry and others – Image not modified from original.
The simplest answer is mutation. The influenza virus is capable of mutating its epitope quite frequently. Unlike other viruses, such as measles, which rarely mutates its epitope, the influenza virus tends to mutate more rapidly and there are many variations of the epitope present in the population at a given time. Furthermore the virus has many subtypes of its epitope, commonly denoted with an H and N. The H represents hemagglutinins and the N refers to neuraminidases both of which are markers on the epitope used to identify the virus. The bird flu scare was denoted as H1N1 corresponding to its specific epitope coating. There are at least 18 hemagglutinins (H1 to H18) and 9 neuraminidases (N1 to N9) that have been found in influenza viruses. Even the same HN virus can differ slightly due to other epitope structure variations, making it nearly impossible for a universal influenza vaccine. So what researchers do instead is to make an educated guess on the strains that will be present during the flu season. They analyze the most prevalent viruses subtypes from patients already sick and choose 4 of those most likely to be infectious in the next flue season. Unfortunately the process of making a vaccine takes around 6 months by which time the virus may have mutated rendering the vaccine less effective. The influenza vaccine is at best 60% effective and at worst is about 10% effective. But the virus may only mutate slightly making the vaccine beneficial in reducing symptoms should an infection occur.
While mutation is the main issue, there are other problems with the creation of the vaccine itself. Chicken eggs are used to grow the flu virus to make the vaccine. Normally, this is not an issue, although except mutations can occur in key places on the viral surface protein hemagglutinin during the growth, which can undermine the effectiveness of shot’s protestation. Using genetically engineered viral proteins instead of chicken eggs could solve this, although this may be more expensive and slower process.
The last issue is with ferrets. I know weird, what do ferrets have to do with a flu vaccine. Well ferrets are, believe it or not, the go to animal model for influenza study, as they are susceptible to both human and avian version of the virus. Unfortunately however, animal models are not identical to humans and can cause discrepancies with the flu vaccine. A possible solution to this would be to also factor in more viral sequence data during vaccination effectiveness and rely less on the ferret model overall.
While the flu vaccine is by no means perfect it saves countless lives by reducing the amount of people getting sick and transmitting the virus. While the flu for most people is a few days of feeling “under the weather”, for the elderly, infants, pregnant women, and other at risk groups, it can be deadly. Although the flu vaccination may not be as perfect as its small pox counterpart was, it still saves people lives and perhaps one day we will find a universal vaccine lifelong vaccine. But until then I would strongly recommend getting vaccinated to protect yourself an others.

Recent Comments